Ovarian cyst
Template:Short description Template:Infobox medical condition (new)
An ovarian cyst is a fluid-filled sac within the ovary.<ref name="womenshealth.gov Ovarian cysts"/> They usually cause no symptoms,<ref name="womenshealth.gov Ovarian cysts"/> but occasionally they may produce bloating, lower abdominal pain, or lower back pain.<ref name="womenshealth.gov Ovarian cysts"/> The majority of cysts are harmless.<ref name="womenshealth.gov Ovarian cysts"/><ref name="OQR dictionary" /> If the cyst either breaks open or causes twisting of the ovary, it may cause severe pain.<ref name="womenshealth.gov Ovarian cysts"/> This may result in vomiting or feeling faint,<ref name="womenshealth.gov Ovarian cysts">Template:Cite web</ref> and even cause headaches.
Most ovarian cysts are related to ovulation, being either follicular cysts or corpus luteum cysts.<ref name="womenshealth.gov Ovarian cysts"/> Other types include cysts due to endometriosis, dermoid cysts, and cystadenomas.<ref name="womenshealth.gov Ovarian cysts"/> Many small cysts occur in both ovaries in polycystic ovary syndrome (PCOS).<ref name="womenshealth.gov Ovarian cysts"/> Pelvic inflammatory disease may also result in cysts.<ref name="womenshealth.gov Ovarian cysts"/> Rarely, cysts may be a form of ovarian cancer.<ref name="womenshealth.gov Ovarian cysts"/> Diagnosis is undertaken by pelvic examination with a pelvic ultrasound or other testing used to gather further details.<ref name="womenshealth.gov Ovarian cysts"/>
Often, cysts are simply observed over time.<ref name="womenshealth.gov Ovarian cysts"/> If they cause pain, medications such as paracetamol (acetaminophen) or ibuprofen may be used.<ref name="womenshealth.gov Ovarian cysts"/> Hormonal birth control may be used to prevent further cysts in those who are frequently affected.<ref name="womenshealth.gov Ovarian cysts"/> However, evidence does not support birth control as a treatment of current cysts.<ref name=Grime2014>Template:Cite journal</ref> If they do not go away after several months, get larger, look unusual, or cause pain, they may be removed by surgery.<ref name="womenshealth.gov Ovarian cysts"/>
Most women of reproductive age develop small cysts each month.<ref name="womenshealth.gov Ovarian cysts"/> Large cysts that cause problems occur in about 8% of women before menopause.<ref name="womenshealth.gov Ovarian cysts"/> Ovarian cysts are present in about 16% of women after menopause, and, if present, are more likely to be cancerous.<ref name="womenshealth.gov Ovarian cysts"/><ref name="ReferenceA">Template:Cite journal</ref> Template:TOC limit
Signs and symptoms

Ovarian cysts tend to produce non-specific symptoms (i.e., symptoms that could be caused by a large number of conditions).<ref name=":0">Template:Citation</ref> Some or all of the following symptoms may be present, though it is possible not to experience any symptoms:<ref name=HELM2013 />
- Abdominal pain. Dull aching pain within the abdomen or pelvis, especially during intercourse.
- Uterine bleeding. Pain during or shortly after beginning or end of menstrual period; irregular periods, or abnormal uterine bleeding or spotting.
- Fullness, heaviness, pressure, swelling, or bloating in the abdomen. Some ovarian cysts become large enough to cause the lower abdomen to visibly swell.<ref name="OQR dictionary" />
- When a cyst ruptures from the ovary, there may be sudden and sharp pain in the lower abdomen on one side.
- Large cysts can cause a change in frequency or ease of urination (such as inability to fully empty the bladder), or difficulty with bowel movements due to pressure on adjacent pelvic anatomy.<ref name=":0" />
- Constitutional symptoms such as fatigue, headaches.
- Nausea or vomiting
- Weight gain
Other symptoms may depend on the cause of the cysts:<ref name=HELM2013 />
- Symptoms that may occur if the cause of the cysts is polycystic ovarian syndrome (PCOS) may include increased facial hair or body hair, acne, obesity and infertility.
- If the cause is endometriosis, then periods may be heavy, and intercourse painful.
The effect of cysts not related to PCOS on fertility is unclear.<ref>Template:Cite journal</ref>
In other cases, the cyst is asymptomatic, and is discovered incidentally while doing medical imaging for another condition.<ref name="Tsili 2020">Template:Cite journal</ref> Ovarian cysts and other "incidentalomas" of the uterine adnexa appear in almost 5% of CT scans done on women.<ref name="Tsili 2020" />
Complications
The most common complications are cyst rupture, which occasionally leads to internal bleeding ("hemorrhagic cyst"), and ovarian torsion.<ref name=":0" />
Cyst rupture
When the surface of cyst breaks, the contents can leak out; this is called a ruptured cyst. The main symptom is abdominal pain, which may last a few days to several weeks, but they can also be asymptomatic.<ref>Template:EMedicine</ref>
A ruptured ovarian cyst is usually self-limiting, and only requires keeping an eye on the situation and pain medications for a few days, while the body heals itself.<ref name=":0" /> Rupture of large ovarian cysts can cause bleeding inside the abdominal cavity.<ref name=":0" /> Rarely, enough blood will be lost that the bleeding will produce hypovolemic shock, which can be a medical emergency requiring surgery.<ref name=":0" /><ref>Template:Cite web</ref> However, normally, the internal bleeding is minimal and requires no intervention.<ref name=":0" />
Ovarian torsion
Ovarian torsion is a very painful medical condition requiring urgent surgery.<ref name="OQR dictionary" /> It can be caused by a pedunculated ovarian cyst that twisted in a way that cuts off the blood flow.<ref name="OQR dictionary" /> It is most likely to be seen in women of reproductive age, though it has happened in young girls (premenarche) and postmenopausal women.<ref name="Mettler 2020">Template:Citation</ref> Ovarian torsion may be more likely during pregnancy, especially during the third and fourth months of pregnancy, as the internal anatomy shifts to accommodate fetal growth.<ref name=":0" /> Diagnosis relies on clinical examination and ultrasound imaging.<ref name=":0" />
Cysts larger than 4 cm are associated with approximately 17% risk.Template:Citation needed
Types

There are many types of ovarian cysts, some of which are normal and most of which are benign (non-cancerous).<ref name="OQR dictionary" />
Functional
Functional cysts form as a normal part of the menstrual cycle. There are several types of functional cysts:
- Follicular cyst, the most common type of ovarian cyst.<ref name="OQR dictionary">Template:Cite dictionary</ref> In menstruating women, an ovarian follicle containing the ovum (an unfertilized egg) normally releases the ovum during ovulation.<ref name="OQR dictionary" /> If it does not release the ovum, a follicular cyst of more than 2.5 cm diameter may result.<ref name=HELM2013 /> A ruptured follicular cyst can be painful.<ref name="OQR dictionary" />
- A luteal cyst is a cyst that forms after ovulation, from the corpus luteum (the remnant of the ovarian follicle, after the ovum has been released).<ref name="OQR dictionary" /> A luteal cyst is twice as likely to appear on the right side.<ref name="OQR dictionary" /> It normally resolves during the last week of the menstrual cycle.<ref name="OQR dictionary" /> A corpus luteum that is more than 3 cm is abnormal.<ref name=HELM2013 /><ref name="Tsili 2020" />
- Theca lutein cysts occur within the thecal layer of cells surrounding developing oocytes. Under the influence of excessive hCG, thecal cells may proliferate and become cystic. This is usually on both ovaries.<ref name=HELM2013 />
Non-functional
Non-functional cysts may include the following:
- An ovary with many cysts, which may be found in normal women, or within the setting of polycystic ovary syndrome
- Cysts caused by endometriosis, known as chocolate cysts
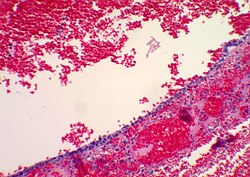
- Hemorrhagic ovarian cyst
- Dermoid cyst – the most common non-functional ovarian cyst, especially for women under the age of 30,<ref name="Mettler 2020" /> they are benign (non-cancerous) with varied morphology.<ref name="Bean 2020">Template:Citation</ref> They can usually be diagnosed from ultrasound alone.<ref name="Bean 2020" /> Depending on size, growth rate (usually slow), and the age of the woman, treatment might involve surgical removal or watchful waiting.<ref name="Bean 2020" /> They are also called mature cystic teratomas.<ref name="Mettler 2020" />
- Ovarian serous cystadenoma – more common in women between the age of 30 and 40.<ref name="Mettler 2020" />
- Ovarian mucinous cystadenoma – although there is usually only one of these, they can grow very large, with diameters sometimes exceeding 50 cm (20 inches).<ref name="Mettler 2020" />
- Paraovarian cyst
- Cystic adenofibroma
- Borderline tumoral cysts
-
Transvaginal ultrasonography of a hemorrhagic ovarian cyst, probably originating from a corpus luteum cyst. The coagulating blood gives the content a cobweb-like appearance.
-
Transvaginal ultrasonography showing a 67 x 40 mm endometrioma, with a somewhat grainy content
Risk factors
Risk factors include fertility status (more common in women of childbearing age) and irregular menstrual cycles.<ref name=":1">Template:Citation</ref> Using combined hormonal contraception may reduce the risk, especially with high-dose pills,<ref name=":1" /> but it does not treat existing cysts.<ref name="Grime2014" />
Diagnosis


Ovarian cysts are usually diagnosed by pelvic ultrasound, CT scan, or MRI, and correlated with clinical presentation and endocrinologic tests as appropriate.<ref name=MedlinePlusEncyclopedia001504>Template:MedlinePlusEncyclopedia</ref> Ultrasound is the most important imaging modality, as abnormalities seen in a CT scan sometimes prove to be normal in ultrasound.<ref name=":0" /><ref name="Tsili 2020" /> If a different modality is needed, then MRIs are more reliable than CT scans.<ref name=":0" />
Ultrasound
Usually, an experienced sonographer can readily identify benign ovarian cysts, often with a level of accuracy that rivals other approaches.<ref name=":0" />
Follow-up imaging in women of reproductive age for incidentally discovered simple cysts on ultrasound is not needed until 5 cm, as these are usually normal ovarian follicles. Simple cysts 5 to 7 cm in premenopausal females should be followed yearly. Simple cysts larger than 7 cm require further imaging with MRI or surgical assessment. Because they are large, they cannot be reliably assessed by ultrasound alone; it can be difficult to see posterior wall soft tissue nodularity or thickened septation due to limited ultrasound beam penetrance at this size and depth. For the corpus luteum, a dominant ovulating follicle that typically appears as a cyst with circumferentially thickened walls and crenulated inner margins, follow up is not needed if the cyst is less than 3 cm in diameter.<ref name="Tsili 2020" /> In postmenopausal women, any simple cyst greater than 1 cm but less than 7 cm needs yearly follow-up, while those greater than 7 cm need MRI or surgical evaluation, similar to reproductive age females.<ref name="levine1">Template:Cite journal</ref>

For incidentally discovered dermoids, diagnosed on ultrasound by their pathognomonic echogenic fat, either surgical removal or yearly follow up is indicated, regardless of the woman's age. For peritoneal inclusion cysts, which have a crumpled tissue-paper appearance and tend to follow the contour of adjacent organs, follow up is based on clinical history. Hydrosalpinx, or fallopian tube dilation, can be mistaken for an ovarian cyst due to its anechoic appearance. Follow-up for this is also based on clinical presentation.<ref name="levine1"/>
For multilocular cysts with thin septation less than 3 mm, surgical evaluation is recommended. The presence of multiloculation suggests a neoplasm, although the thin septation implies that the neoplasm is benign. For any thickened septation, nodularity, vascular flow on color doppler, or growth over several ultrasounds, surgical removal may be considered due to concern of cancer.<ref name="levine1"/>
Scoring systems
Most ovarian cysts are not malignant; however, some do become cancerous.<ref name="OQR dictionary" /> There are several systems to assess risk of an ovarian cyst of being an ovarian cancer, including the RMI (risk of malignancy index), LR2 and SR (simple rules). Sensitivities and specificities of these systems are given in tables below:<ref name="KaijserSayasneh2013">Template:Cite journal</ref>
| Scoring systems | Premenopausal | Postmenopausal | ||
|---|---|---|---|---|
| Sensitivity | Specificity | Sensitivity | Specificity | |
| RMI I | 44% | 95% | 79% | 90% |
| LR2 | 85% | 91% | 94% | 70% |
| SR | 93% | 83% | 93% | 76% |
Ovarian cysts may be classified according to whether they are a variant of the normal menstrual cycle, referred to as a functional or follicular cyst.<ref name=HELM2013>Template:EMedicine</ref>
Ovarian cysts are considered large when they are over 5 cm and giant when they are over 15 cm. In children, ovarian cysts reaching above the level of the umbilicus are considered giant.
Associated conditions
In juvenile hypothyroidism multicystic ovaries are present in about 75% of cases, while large ovarian cysts and elevated ovarian tumor marks are one of the symptoms of the Van Wyk and Grumbach syndrome.<ref name=Durbin_2011>Template:Cite journal</ref>
The CA-125 marker in children and adolescents can be frequently elevated even in absence of malignancy and conservative management should be considered.
Polycystic ovarian syndrome involves the development of multiple small cysts in both ovaries due to an elevated ratio of leutenizing hormone to follicle stimulating hormone, typically more than 25 cysts in each ovary, or an ovarian volume of greater than 10 mL.<ref>Template:Cite journal</ref>
Larger bilateral cysts can develop as a result of fertility treatment due to elevated levels of HCG, as can be seen with the use of clomifene for follicular induction, in extreme cases resulting in a condition known as ovarian hyperstimulation syndrome.<ref>Template:Cite journal</ref> Certain malignancies can mimic the effects of clomifene on the ovaries, also due to increased HCG, in particular gestational trophoblastic disease. Ovarian hyperstimulation occurs more often with invasive moles and choriocarcinoma than complete molar pregnancies.<ref>Template:Cite journal</ref>
Risk of cancer
Accurately differentiating an cyst from a cancer is critical to management. Medical imaging showing a simple, smooth bubble of watery liquid is characteristic of a benign cyst.<ref name="Tsili 2020" /> If the cyst is large, is multilocular, or has complex internal features, such as papillary (bumpy) projections into the cyst or solid areas inside the cyst, it is more likely to be cancerous.<ref name="Bean 2020" />
A widely recognised method of estimating the risk of malignant ovarian cancer based on initial workup is the risk of malignancy index (RMI).<ref name="Bean 2020" /><ref name="NICE2011">NICE clinical guidelines Issued: April 2011. Guideline CG122. Ovarian cancer: The recognition and initial management of ovarian cancer Template:Webarchive, Appendix D: Risk of malignancy index (RMI I).</ref> It is recommended that women with an RMI score over 200 should be referred to a centre with experience in ovarian cancer surgery.<ref name="sign2003">Template:Cite book</ref>
The RMI is calculated as follows:<ref name="sign2003"/>
- RMI = ultrasound score × menopausal score × CA-125 level in U/ml.
There are two methods to determine the ultrasound score and menopausal score, with the resultant RMI being called RMI 1 and RMI 2, respectively, depending on what method is used:<ref name="sign2003"/>
| Feature | RMI 1 | RMI 2 |
|---|---|---|
|
Ultrasound abnormalities:
|
Template:Plainlist | Template:Plainlist |
| Menopausal score | Template:Plainlist | Template:Plainlist |
| CA-125 | Quantity in U/ml | Quantity in U/ml |
RMI 2 is regarded as more sensitive than RMI 1,<ref name="sign2003" /> but the model has low specificity, which means that many of the suspected cancers turn out to be overdiagnosed benign cysts.<ref name="Bean 2020" /> The calculation is often inaccurate during pregnancy, especially when CA-125 levels peak towards the end of the first trimester.<ref name=":0" />
The International Ovarian Tumor Analysis (IOTA) group has produced a different model. Theirs relies on "simple descriptors" and "simple rules".<ref name=":0" /> An example of a simple descriptor for a benign cyst is "Unilocular cyst of anechoic content with regular walls and largest diameter less than 10 cm".<ref name=":0" /> An example of a simple rule is acoustic shadows are associated with benign cysts.<ref name=":0" />
Histopathology
In case an ovarian cyst is surgically removed, a more definite diagnosis can be made by histopathology:
| Type | Subtype | Typical microscopy findings | Image |
|---|---|---|---|
| Functional cyst | Follicular cyst |
|

|
| Corpus luteum cyst |
|
| |
| Cystadenoma | Serous cystadenoma | Cyst lining consisting of a simple epithelium, whose cells may be either:<ref>Template:Cite web Topic Completed: 1 June 2012. Revised: 5 March 2020</ref>
|

|
| Mucinous cystadenoma | Lined by a mucinous epithelium | 
| |
| Dermoid cyst | Well-differentiated components from at least two, and usually three,<ref name="Mettler 2020" /> germ layers (ectoderm, mesoderm and/or endoderm).<ref name="SahinAbdullazade2017">Template:Cite journal</ref> | 
| |
| Endometriosis | At least two of the following three criteria:<ref>Template:Cite web Topic Completed: 1 August 2017. Revised: 5 March 2020</ref>
|

| |
| Borderline tumor | Atypical epithelial proliferation without stromal invasion.<ref>Template:Cite web This topic last updated: Feb 08, 2019.</ref> | 
| |
| Ovarian cancer | Many different types, but generally severe dysplasia/atypia and invasion. | 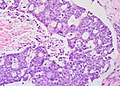
| |
| Simple squamous cyst | Simple squamous epithelium and not conforming to diagnoses above (a diagnosis of exclusion) | 
| |
Treatment
Most ovarian cysts occur naturally and go away in a few months without needing any treatment.<ref name="nhs2023oc">Template:OGL-attribution</ref> In general, there are three options for dealing with an ovarian cyst:
- watchful waiting (e.g., waiting to see whether symptoms resolve on their own),<ref name="Tsili 2020" />
- additional imaging or investigation (e.g., getting an ultrasound later to see whether the cyst is growing),<ref name="Tsili 2020" /> and
- surgery (e.g., surgical removal of the cyst).<ref name="Tsili 2020" />
Cysts associated with hypothyroidism or other endocrine problems are managed by treating the underlying condition.
About 95% of ovarian cysts are benign (not cancerous).<ref>Template:Cite web</ref> Functional cysts and hemorrhagic ovarian cysts usually resolve spontaneously within one or two menstrual cycles.<ref name="Mettler 2020" />
However, the bigger an ovarian cyst is, the less likely it is to disappear on its own.<ref name="Bluth2000">Template:Cite book</ref> Treatment may be required if cysts persist over several months, grow, or cause increasing pain.<ref name="Orshan2008">Template:Cite book</ref> Cysts that persist beyond two or three menstrual cycles, or occur in post-menopausal women, may indicate more serious disease and should be investigated through ultrasonography and laparoscopy, especially in cases where family members have had ovarian cancer. Such cysts may require surgical biopsy. Additionally, a blood test may be taken before surgery to check for elevated CA-125, a tumour marker, which is often found in increased levels in ovarian cancer, although it can also be elevated by other conditions resulting in a large number of false positives.<ref>Template:MedlinePlusEncyclopedia</ref>
Expectant management
If the cyst is asymptomatic and appears to be either benign or normal (i.e., a cyst with a benign appearance and a size of less than 3 cm diameter in premenopausal women or less than 1 cm in postmenopausal women<ref name="Tsili 2020" />), then delaying surgery, in the hope that it will prove unnecessary, is appropriate and recommended.<ref name="Tsili 2020" /> Normal ovarian cysts require neither treatment nor additional investigations.<ref name="Tsili 2020" /> Benign but medium-size cysts may prompt an additional pelvic ultrasound after a couple of months.<ref name="Tsili 2020" /> (The larger the cyst, the sooner the follow-up imaging is done.<ref name="Tsili 2020" />)
Symptom management Template:Anchor
Pain associated with ovarian cysts may be treated in several ways:
- Pain relievers such as acetaminophen, nonsteroidal anti-inflammatory drugs,<ref name="womenshealth.gov Ovarian cysts"/> or opioids.
- While hormonal birth control prevents the development of new cysts in those who frequently get them,<ref name="womenshealth.gov Ovarian cysts"/> it is not useful for the treatment of current cysts.<ref name=Grime2014/>
Surgery
Template:See also Although most cases of ovarian cysts are monitored and stabilize or resolve without surgery, some cases require surgery.<ref>Template:Cite book</ref> Common indications for surgical management include ovarian torsion, ruptured cyst, concerns that the cyst is cancerous, and pain;<ref name="Mettler 2020" /> some surgeons additionally recommend removing all large cysts.<ref name="Mettler 2020" />
The surgery may involve removing the cyst alone, or one or both ovaries.<ref name="Mettler 2020" /> Very large, potentially cancerous, and recurrent cysts, particularly in menopausal women, are more likely to be treated by removing the affected ovary, or both the ovary and its Fallopian tube (salpingo-oophorectomy).<ref name="Mettler 2020" /> For women of reproductive age, the aim is to preserve as much of the reproductive system as possible. It's often possible to just remove the cyst and leave both ovaries intact, which means the fertility should be unaffected.<ref name="c157" />
Simple benign cysts can be drained through fine-needle aspiration.<ref name=":0" /> However, the risk of recurrence is fairly high (33–40%), and if a cancerous tumor was misdiagnosed, it could cause the cancer to spread.<ref name=":0" />
The surgical technique is typically a minimally invasive or laparoscopic approach performed under general anaesthesia,<ref name="Mettler 2020" /> unless the cyst is particularly large (e.g., 10 cm [4 inches] in diameter), or if pre-operative imaging, such as pelvic ultrasound, suggests malignancy or complex anatomy.<ref name="Bean 2020" /> For large cysts, open laparotomy or a mini-laparotomy (a smaller incision through the abdominal wall) may be preferred.<ref name="Bean 2020" /> Minimally invasive surgeries are not used when ovarian cancer is suspected.<ref name="Bean 2020" /><ref name="Mettler 2020" /> Additionally, if the pelvic surgery is being done, some women choose to have prophylactic salpingectomy done at the same time, to reduce their future risk of cancer.<ref name="Mettler 2020" />
If the cyst ruptures during surgery, the contents may irritate the peritoneum and cause internal adhesions.<ref name="Mettler 2020" /> The cyst may be drained before removal, and the abdominal cavity carefully irrigated to remove any leaked fluids, to reduce this risk.<ref name="Mettler 2020" />
After surgery
The time it takes to recover from surgery is different for everyone. After the ovarian cyst has been removed, one will feel pain in the tummy, although this should improve in a few days.<ref name="c157">Template:OGL-attribution</ref>
After a laparoscopy or a laparotomy, it may take as long as 12 weeks before one can resume normal activities.<ref name="c157" /> If the cyst is sent off for testing, the results should come back in a few weeks. These symptoms may indicate an infection and need further attention:<ref name="c157" />
- heavy bleeding
- severe pain or swelling in the abdomen
- a high temperature (fever)
- dark or smelly vaginal discharge<ref name="c157" />
Cancer treatment
If the test results show that the cyst is cancerous, both ovaries, the uterus, and some of the surrounding tissue may need to be removed. This would trigger an early menopause and means that pregnancy is no longer possible.<ref name="c157" />
Treating conditions that cause ovarian cysts
If a condition that can cause ovarian cysts, such as endometriosis or polycystic ovary syndrome (PCOS), has been diagnosed, treatment may be different.<ref name="c157" /> For example, endometriosis may be treated with painkillers, hormone medication, and/or surgery to remove or destroy areas of endometriosis tissue.<ref name="c157" />
Frequency
Most women of reproductive age develop small cysts each month. Simple, smooth ovarian cysts, smaller than 3 cm and apparently filled with water, are considered normal.<ref name="Tsili 2020" /> Large cysts that cause problems occur in about 8% of women before menopause.<ref name="womenshealth.gov Ovarian cysts"/> Ovarian cysts are present in about 16% of women after menopause, and have a higher risk of being cancer than in younger women.<ref name="womenshealth.gov Ovarian cysts"/><ref name="ReferenceA"/> If a cyst appears benign during diagnosis, then it has a less than 1% chance of being either cancer or borderline malignant.<ref name="Mettler 2020" />
Benign ovarian cysts are common in asymptomatic premenarchal girls and found in approximately 68% of ovaries of girls 2–12 years old and in 84% of ovaries of girls 0–2 years old. Most of them are smaller than 9 mm while about 10–20% are larger macrocysts. While the smaller cysts mostly disappear within 6 months the larger ones appear to be more persistent.<ref name=Cohen_1992>Template:Cite journal</ref><ref name=Qublan_2010>Template:Cite journal</ref>
In pregnancy
Ovarian cysts are seen during pregnancy.<ref name=":1" /><ref name=":0" /> They tend to be simple benign cysts measuring less than 5 cm in diameter, most commonly functional follicular or luteal cysts.<ref name=":1" /> They are more common earlier in the pregnancy.<ref name=":0" /> When they are detected early in pregnancy, such as during a routine prenatal ultrasound, they usually resolve on their own after a couple of months.<ref name=":1" /><ref name=":0" /> Pregnancy changes hormone levels, and that can affect the diagnostic process.<ref name=":0" /> For example, some endometriomas (a type of benign ovarian cyst) will undergo decidualization, which can make them look more like a cancerous tumor in medical imaging.<ref name=":0" />
A large cyst, if it puts pressure on the lower part of the uterus, can cause obstructed labor (also called labor dystocia).<ref name=":0" />
Rarely, a cyst discovered during pregnancy will prove to be cancerous or to have cancerous potential.<ref name=":0" /> Malignant tumors discovered during pregnancy are usually germ cell, sex cord–gonadal stromal, or carcinomas, or slightly less commonly, borderline serous or mucinous cysts.<ref name=":0" />
History
In 1809, Ephraim McDowell became the first surgeon to successfully remove an ovarian cyst.<ref>Template:Cite book</ref>
Society and culture
Benign tumors were known in ancient Egypt, and an ovarian cyst has been identified in a mummy, Irtyersenu (c. 600 BC), that was autopsied in the early 19th century.<ref>Template:Cite book</ref>

