Trigeminal neuralgia
Template:Short description Template:Cs1 config Template:Infobox medical condition (new)
Trigeminal neuralgia (TN or TGN), also called Fothergill disease, tic douloureux, or trifacial neuralgia, is a long-term pain disorder that affects the trigeminal nerve,<ref>Template:Cite web</ref><ref name=NIH2015>Template:Cite web</ref> the nerve responsible for sensation in the face and motor functions such as biting and chewing. It is a form of neuropathic pain.<ref name=":0">Template:Cite journal</ref> There are two main types: typical and atypical trigeminal neuralgia.<ref name=NIH2015/>
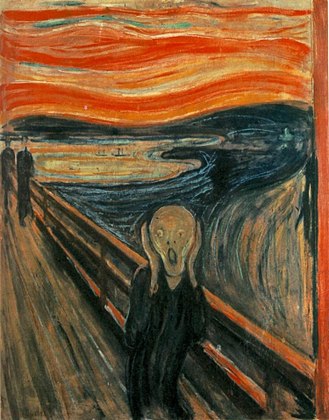
The typical form results in episodes of severe, sudden, shock-like pain in one side of the face that lasts for seconds to a few minutes. Groups of these episodes can occur over a few hours. The atypical form results in a constant burning pain that is less severe. Episodes may be triggered by any touch to the face.<ref name=NIH2015/> Both forms may occur in the same person. Pain from the disease has been linked to mental-health issues, especially depression.<ref name=Okeson2005>Template:Cite book</ref>
The exact cause is unknown, but believed to involve loss of the myelin of the trigeminal nerve.<ref name="Ob2010" /> This might occur due to nerve compression from a blood vessel as the nerve exits the brain stem, multiple sclerosis, stroke, or trauma. Less common causes include a tumor or arteriovenous malformation. It is a type of nerve pain. Diagnosis is typically based on the symptoms, after ruling out other possible causes such as postherpetic neuralgia.<ref name=":0" /><ref name="NIH2015" />
Treatment includes medication or surgery. The anticonvulsant carbamazepine or oxcarbazepine is usually the initial treatment, and is effective in about 90% of people.<ref name=":0" /> Side effects are frequently experienced that necessitate drug withdrawal in as many as 23% of patients.<ref name=":0" /> Other options include lamotrigine, baclofen, gabapentin, amitriptyline, and pimozide.<ref name=Ob2010/> Opioids are not usually effective in the typical form. In those who do not improve or become resistant to other measures, a number of types of surgery may be tried.<ref name=Ob2010>Template:Cite journal</ref><ref name=NIH2015/>
Trigeminal neuralgia affects an estimated 0.03% to 0.30% of people around the world, with a 3:1 ratio between women and men.<ref>Template:Cite journal</ref> It usually begins in people over 50 years old, but can occur at any age.<ref name=NIH2015/> The condition was first described in detail in 1773 by John Fothergill.<ref>Template:Cite journal</ref> Template:TOC limit
Signs and symptoms

This disorder is characterized by episodes of severe facial pain along the trigeminal nerve divisions. The trigeminal nerve is a paired cranial nerve that has three major branches - the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3). Any or all branches of the nerve may be affected. Trigeminal neuralgia most commonly involves the middle branch (the maxillary nerve or V2) and lower branch (mandibular nerve or V3) of the trigeminal nerve.<ref>Template:Cite web</ref>
An individual attack usually lasts from a few seconds to several minutes or hours, but these can repeat for hours with very short intervals between attacks. In other instances, only four to 10 attacks are experienced daily. The episodes of intense pain may occur paroxysmally. To describe the pain sensation, people often describe a trigger area on the face so sensitive that touching or even air currents can trigger an episode, but in many people, the pain is generated spontaneously without any apparent stimulation.
It affects lifestyle, as it can be triggered by common activities such as eating, talking, shaving, and brushing teeth. The wind, chewing, and talking can aggravate the condition in many patients. The attacks are said, by those affected, to feel like stabbing electric shocks, burning, sharp, pressing, crushing, exploding, or shooting pain that becomes intractable.<ref name=":0" />
The pain also tends to occur in cycles with remissions lasting months or even years. Pain attacks are known to worsen in frequency or severity over time in some people. Pain may migrate to other branches over time, but in some people remains very stable.<ref name="Bayer1979">Template:Cite journal</ref>
Bilateral (occurring on both sides) trigeminal neuralgia is very rare except for trigeminal neuralgia caused by multiple sclerosis (MS). This normally indicates problems with both trigeminal nerves, since one nerve serves the left side of the face and the other serves the right side. Occasional reports of bilateral trigeminal neuralgia reflect successive episodes of unilateral (only one side) pain switching the side of the face rather than pain occurring simultaneously on both sides.<ref>Template:Cite journal</ref>
Rapid spreading of the pain, bilateral involvement, or simultaneous participation with other major nerve trunks (such as painful tic convulsive of nerves V and VII or occurrence of symptoms in the V and IX nerves) may suggest a systemic cause. Systemic causes could include MS or expanding cranial tumors.<ref name="Okeson 2005 453">Template:Cite book</ref>
The severity of the pain makes washing the face, shaving, and performing good oral hygiene more difficult. The pain has a significant impact on activities of daily living, especially as those affected live in fear of when they are going to get their next attack of pain and how severe it will be. It can lead to severe depression and anxiety.<ref name="SmithElias2013">Template:Cite journal</ref>
Not all people, though, have the symptoms described above; several variants of TN occur, one of which is atypical trigeminal neuralgia (trigeminal neuralgia, type 2 or trigeminal neuralgia with concomitant pain),<ref name=OHSU>Template:Cite web</ref> based on a recent classification of facial pain.<ref name=Burchiel2003>Template:Cite journal</ref> In these instances, a more prolonged, lower-severity background pain can be present for over 50% of the time and is described more as a burning or prickling, rather than a shock.
Trigeminal pain can also occur after an attack of herpes zoster. Postherpetic neuralgia has the same manifestations as in other parts of the body. Herpes zoster oticus typically presents with inability to move many facial muscles, pain in the ear, taste loss on the front of the tongue, dry eyes and mouth, and a vesicular rash. Less than 1% of varicella zoster infections involve the facial nerve and result in this occurring.<ref>Template:Cite journal</ref>
Trigeminal deafferentation pain (TDP), also termed anesthesia dolorosa, or colloquially as phantom face pain, is from unintentional damage to a trigeminal nerve following attempts to fix a nerve problem surgically. TDP is usually constant with a burning sensation and numbness and is very difficult to treat, as further surgeries are usually ineffective and possibly detrimental to the person.<ref>Template:Cite web</ref>
Causes
Template:See also The trigeminal nerve is a mixed cranial nerve responsible for sensory data such as tactition (pressure), thermoception (temperature), and nociception (pain) originating from the face above the jawline; it is also responsible for the motor function of the muscles of mastication (those involved in chewing but not facial expression).<ref>Template:Cite web</ref>
Several theories exist to explain the possible causes of this pain syndrome. The nerve was once thought to be compressed in the opening from the inside to the outside of the skull; but leading research indicates that it is an enlarged or lengthened blood vessel – most commonly the superior cerebellar artery – compressing or throbbing against the microvasculature of the trigeminal nerve near its connection with the pons.<ref>Template:Cite journal</ref> Such a compression can injure the nerve's protective myelin sheath and cause erratic and hyperactive functioning of the nerve. This can lead to pain attacks at the slightest stimulation of any area served by the nerve, as well as hindering the nerve's ability to shut off the pain signals after the stimulation ends. This type of injury may rarely be caused by an aneurysm (an outpouching of a blood vessel), by an arteriovenous malformation,<ref name="SinghBharatha2014">Template:Cite journal</ref> by a tumor; such as an arachnoid cyst or meningioma in the cerebellopontine angle;<ref name=Babu1991>Template:Cite journal</ref> or by a traumatic event, such as a car accident.<ref>Template:Cite book</ref>
Short-term peripheral compression is often painless.<ref name=Okeson2005/> Persistent compression results in local demyelination with no loss of axon potential continuity. Chronic nerve entrapment results in demyelination primarily, with progressive axonal degeneration subsequently.<ref name=Okeson2005/> It is, "therefore widely accepted that trigeminal neuralgia is associated with demyelination of axons in the Gasserian ganglion, the dorsal root, or both."<ref name="Okeson 2005 115">Template:Cite book</ref> This compression may be related to an aberrant branch of the superior cerebellar artery that lies on the trigeminal nerve.<ref name="Okeson 2005 115"/> Further causes, besides an aneurysm, MS, or cerebellopontine angle tumor, include a posterior fossa tumor, any other expanding lesion, or even brainstem diseases from strokes.<ref name="Okeson 2005 115"/>
Trigeminal neuralgia is found in 3–4% of people with MS, according to data from seven studies.<ref>Template:Cite journal</ref><ref>Template:Cite journal</ref> This is theorized to be due to damage to the spinal trigeminal complex.<ref name=Cruccu2009>Template:Cite journal</ref> Trigeminal pain has a similar presentation in patients with and without MS.<ref name=Simone2005>Template:Cite journal</ref>
Postherpetic neuralgia, which occurs after shingles, may cause similar symptoms if the trigeminal nerve is damaged, called Ramsay Hunt syndrome type 2.
When no structural cause is apparent, the syndrome is called idiopathic TN.
Diagnosis
Trigeminal neuralgia is diagnosed by the result of neurological and physical tests, as well as the individual's medical history.<ref name="NIH2015"/> Magnetic resonance angiography can be used to detect vascular compression of the trigeminal nerve and refer patients to surgery.<ref>Template:Cite journal</ref>
As with many conditions without clear physical or laboratory diagnoses, TN is often misdiagnosed, and other conditions are also frequently misdiagnosed as TN.<ref name=":1">Template:Cite journal</ref><ref>Template:Cite journal</ref> A person with TN may see three or four clinicians before a firm diagnosis is made.<ref name=":1" />
Temporomandibular disorder (TMD) can present similarly to TN; differentiating between these conditions can be difficult.<ref name="Drangsholt2001">Template:Cite journal</ref> Even suspected TN patients who experience brief attacks of sharp pain have had their symptoms resolve after being treated for TMD.<ref>Template:Cite journal</ref> TMD pain can also be triggered by movements of the tongue or facial muscles, so TN must be differentiated from masticatory pain by differentiating between the clinical characteristics of deep somatic pain and neuropathic pain. Masticatory pain will not be arrested by a conventional mandibular local anesthetic block.<ref name="Okeson 2005 453" /> One quick test a dentist might perform is a conventional inferior dental local anesthetic block. If the pain is in the treated branch, the block will not arrest masticatory pain but will alleviate TN pain.<ref>Template:Cite web</ref>
Management
Some evidence points towards the need to quickly treat and diagnose TN. The longer a patient has TN, reversing the neural pathways associated with the pain are thought to be more difficult.Template:Citation needed
Medical
- The anticonvulsant carbamazepine is the first-line treatment; second-line medications include baclofen, lamotrigine, oxcarbazepine, phenytoin, topiramate, gabapentin, and pregabalin. Uncontrolled trials have suggested that clonazepam and lidocaine may be effective.<ref name=Sindrup2002>Template:Cite journal</ref>
- Antidepressant medications, such as amitriptyline, have shown good efficacy in treating TN, especially if combined with an anticonvulsant drug such as pregabalin.<ref>Template:Cite journal</ref>
- Some evidence indicates that duloxetine can also be used in some cases of neuropathic pain, especially in patients with major depressive disorder,<ref>Template:Cite journal</ref> as it is an antidepressant. By no means, though, should it be considered a first-line therapy and should only be tried by specialist's advice.<ref>Template:Cite journal</ref>
- Controversy exists around opiate use such as morphine and oxycodone for treatment of TN, with varying evidence on its effectiveness for neuropathic pain. Generally, opioids are considered ineffective against TN, thus should not be prescribed.<ref>Template:Cite journal</ref>
Surgical
Microvascular decompression provides freedom from pain in about 75% of patients presenting with drug-resistant TN.<ref>Template:Cite journal</ref><ref name=Surgery11>Template:Cite journal</ref><ref>Template:Cite web</ref> While there may be pain relief after surgery, there is also a risk of adverse effects, such as facial numbness. Percutaneous radiofrequency thermorhizotomy may also be effective<ref name="Sindou 203–10">Template:Cite journal</ref> as may stereotactic radiosurgery; however the effectiveness decreases with time.<ref>Template:Cite journal</ref>
Surgical procedures can be separated into nondestructive and destructive:
Nondestructive
- Microvascular decompression involves a small incision behind the ear and some bone removal from the area. An incision through the meninges is made to expose the nerve. Any vascular compressions of the nerve are carefully moved and a sponge-like pad is placed between the compression and nerve, stopping unwanted pulsation and allowing myelin sheath healing.Template:Citation needed
Destructive
All destructive procedures cause facial numbness after relief, as well as pain relief.<ref name="Surgery11"/>
- Percutaneous techniques, which all involve a needle or catheter entering the face up to the origin where the nerve splits into three divisions and then damaging this area, purposely, produce numbness, but also stop pain signals. These techniques are proven effective,<ref name="Sindou 203–10"/> especially in those where other interventions have failed or in those who are medically unfit for surgery, such as the elderly.
- Balloon compression uses inflation of a balloon at this point, causing damage and stopping pain signals.
- Glycerol injection, deposition of corrosive liquid glycerol at this point, causes damage to the nerve to hinder pain signals.
- Radiofrequency thermocoagulation rhizotomy is the application of a heated needle to damage the nerve at this point.
- Stereotactic radiosurgery is a form of radiation therapy that focuses high-power energy on a small area of the body.<ref>Template:Cite web</ref>
Support
Psychological and social support have been found to play a key role in the management of chronic illnesses and chronic pain conditions, such as TN. Chronic pain can cause constant frustration to individuals and those around them.<ref>Template:Cite web</ref>
History
Trigeminal neuralgia was first described by physician John Fothergill and treated surgically by John Murray Carnochan, both of whom were graduates of the University of Edinburgh Medical School. Historically, TN has been called "suicide disease" due to studies by the pioneering forefather in neurosurgery Harvey Cushing involving 123 cases of TN between 1896 and 1912. In those studies, it produced intense pain, higher rates of suicidal ideation in patients with severe migraines, and links to higher rates of depression, anxiety, and sleep disorders.<ref name="Adams 1043–50">Template:Cite journal</ref><ref>Template:Cite web</ref><ref name=Prasad2009>Template:Cite journal</ref>
Society and culture
Some individuals of note with TN include:
- Four-time British Prime Minister William Gladstone is believed to have had the disease.<ref>Template:Cite journal</ref>
- Entrepreneur and author Melissa Seymour was diagnosed with TN in 2009 and underwent microvascular decompression surgery in a well-documented case covered by magazines and newspapers, which helped to raise public awareness of the illness in Australia. Seymour was subsequently made a Patron of the Trigeminal Neuralgia Association of Australia.<ref>Template:Cite web</ref>
- Salman Khan, an Indian film star, was diagnosed with TN in 2011. He underwent surgery in the US.<ref>Template:Cite web</ref>
- All-Ireland winning Gaelic footballer Christy Toye was diagnosed with the condition in 2013. He spent five months in his bedroom at home, returned for the 2014 season, and lined out in another All-Ireland final with his team.<ref>Template:Cite news</ref>
- Jim Fitzpatrick – former Member of Parliament for Poplar and Limehouse – disclosed he had TN before undergoing neurosurgery. He has openly discussed his condition at parliamentary meetings and is a prominent figure in the TNA UK charity.<ref>Template:Cite news</ref>
- Jefferson Davis – President of the Confederate States of America<ref>Template:Cite web</ref>
- Charles Sanders Peirce – American philosopher, scientist, and father of pragmatism<ref>Template:Cite book</ref>
- Gloria Steinem – American feminist, journalist, and social and political activist<ref name="Gorney">Template:Cite news</ref>
- Anneli van Rooyen, Afrikaans singer-songwriter popular during the 1980s and 1990s, was diagnosed with atypical Tn in 2004. During surgical therapy directed at alleviating the condition performed in 2007, Van Rooyen had permanent nerve damage, resulting in her near-complete retirement from performing.<ref>Template:Cite web</ref>
- H.R., singer of hardcore punk band Bad Brains<ref>Template:Cite news</ref>
- Aneeta Prem, a British author, human rights campaigner, magistrate, and the founder and president of Freedom Charity experienced bilateral TN beginning in 2010, with severe pain and resulting sleep deprivation. Her condition remained undiagnosed until 2017. MVD surgery to ameliorate the pain on the right-hand side was performed at UCHL in December 2019.<ref>Template:Cite webTemplate:Dead link</ref>
- Travis Barker, drummer of rock band Blink-182<ref>Template:Cite web</ref>
- Karel Heřmánek, Czech actor<ref>Template:Cite news</ref>
See also
- Cluster headache
- Microvascular decompression
- Nerve compression syndrome
- Nerve decompression
- Trigeminal trophic syndrome
References
External links
Template:PNS diseases of the nervous system Template:Headache Template:Medical resources Template:Authority control